Move Beyond the Kegel
I remember a ballet class once upon a time. I was around 21 years old and was working on a petite allegro exercise in my company class (small, fast jumps) when I suddenly experienced a small loss of urine. Nothing catastrophic or noticeable to anyone else but me, but it was still a bit of a surprise when it happened. I didn’t mention it to anyone, because I didn’t think it was of importance, and to be honest, was slightly embarrassed. It didn’t happen again that day, but it did happen again from time to time, usually on a fast jumping sequence. I think I just brushed it off as a whatever thing. How could I possibly explain this random occurrence to someone anyway?
Fast forward to 2022, 16 years after the incident, armed with a with a heck of a lot more understanding. I discovered pilates, I studied human movement, and I have had the privilege of learning from wonderful pelvic health therapists (shout out to the magnificent Trish Gipson at The Cheerful Pelvis) over the last few years, which prompted me to dive into my own research/education building project on the pelvic floor as part of my Kinesiology degree at UBC. It is fascinating stuff!!
I know now that what had occurred to me was likely due to hypertonic (tight; high tone) pelvic floor musculature that was unable to maintain support under excess load (the jumping). The muscles of my pelvic floor were fatigued from being chronically overused – over-recruited abdominal muscles, paired with excessive external rotation forces in my hips from the ballet technique and very likely, the overall stress of the job. I also know now that there ARE practitioners who are more than delighted to discuss these issues and that these occurrences happen to young athletes more frequently than you think. Pelvic floor concerns aren’t just for people post-pregnancy or in menopause, although those demographics have a higher rate of occurrence. Lastly, pelvic floor concerns may encompass more than just incontinence. Do you have pain with sex? Issues with constipation? Nagging tailbone pain? A feeling of heaviness in the perineum or vagina? If you are going hmmmm to any of these things, it might be very worth your while to visit a pelvic health Physio with your concerns. I’ll leave some information at the end of this post about where to go next.
In the meantime, let’s get acquainted with the mechanics of “down there”.
Why is the pelvic floor so important?
The pelvic floor muscle complex is the only muscle group in the body capable of giving structural support against gravity for the pelvic organs at rest and with slow, rapid and unpredictable loading (Sapsford, 2004).
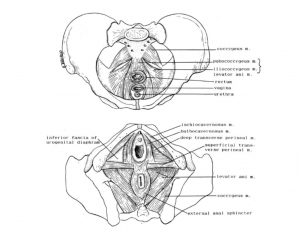
The pelvic floor muscles (PFM) that are typically targeted with pelvic floor muscle training (PFMT) [conscious contractions or “Kegels”] are the pubococcygeus, puborectalis, and iliococcygeus muscles, collectively called the levator ani. They function as a single unit and are considered the deepest layer of the pelvic floor complex (Sapsford, 2004; Bø & Sherburn, 2005). These muscles attach on to various places in the base of the pelvis and provide support and integrity to both the pelvis and the structures above it. See Fig 1.
A contraction of the PFM provides active support for the pelvic organs and maintains continence during changes in intra-abdominal pressure (pressure within your abdominal cavity). It can be described as a squeeze around the pelvic openings and an upward lift.
The relaxation of the PFM is just as important to master as the contraction. Successful urination and defecation, sexual function, and childbirth are all dependent on the PFMs ability to relax effectively. Inability to relax properly can result in pelvic pain and urinary difficulties (Butrick, 2009). Training for relaxation can be considered a “reverse Kegel”.
The relaxation piece is what I had to work on when I finally had my pelvic floor assessed and it seriously made a world of difference. I still have to practice as my tendency is to over-recruit my musculature in general.
Now, this is where you might find things get a bit more interesting, and where we start to see how straight up kegels may not be doing you any favours. Forgive me, Samantha.
The ability for the pelvic floor to contract and to effectively maintain tonic support during movement tasks is dependent on the function of other local muscle groups that contribute to trunk stability (the abdominals and diaphragm) and the alignment of the skeleton (Sapsford, 2004; Grewar & Maclean 2008).
What this means, is that Kegels alone are not enough, or may even be counterproductive to your individual needs. Working Kegels in isolation is also not ideal; it doesn’t correspond effectively to the dynamic, variable movement ability our bodies have. Yes, Kegels (both the contraction and release portions) can be important to develop awareness, and to regulate tone but they aren’t the final answer.
Consider your bicep muscle. Do you tense your bicep continuously without any other movements in order to strengthen it? No. You would work on shortening the muscle under load (bicep curl) and lengthening it under load (releasing bicep curl slowly). You would integrate it into more complex movements (pull ups, cleans) and you would use the biceps with different positioning of your shoulders or lower arm. In essence, the pelvic floor isn’t really all that different, it needs to know how to shorten and lengthen under load and how to react quickly, or with endurance. It needs to be able to coordinate its contractile abilities with other muscle groups and in various body positions for the best outcome for the meaningful task you are after (ie running, jumping, heavy weight lifting).
Lets have a look at regular function of the core unit:
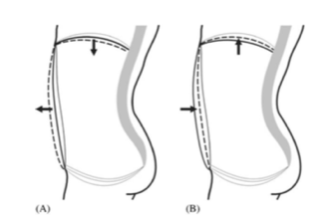
The PFM can be considered the bottom part of the ‘abdominal canister or core’. They work synergistically with the abdominal muscles and thoracic diaphragm to provide trunk stability, respond to changes in intra-abdominal pressure (IAP), which is defined as pressure within the abdominal cavity, and to promote continence (Talasz, Kremser, Kofler, Kalchschmid, Lechleitner, & Rudisch, 2011)
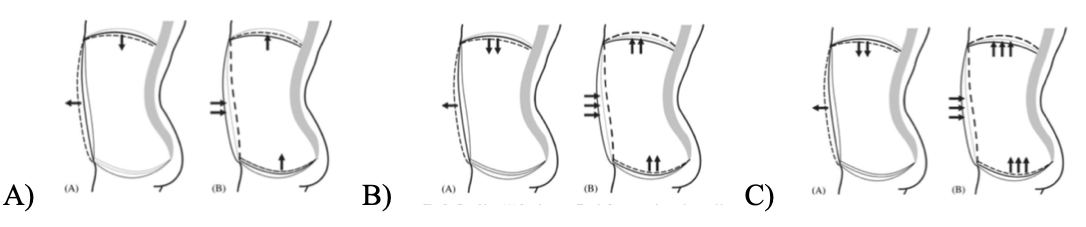
With forced exhalation (cough, sneeze, lifting etc.) The abdomen should pull in harder, the PFM contract strongly and the diaphragm will be forced higher (Fig 3.2). This coordinated pattern acts as a “bellows” that focuses the increase in IAP toward the diaphragm (Talasz et al., 2010;2011). If there are changes to this coordinated effort, for example if tension in the abdominals prevent anterior movement on inhalation, this will change the application of expiration force on the diaphragm and PF and may affect the ability to maintain continence. Focusing on the mechanics of breathing first will support the training of the deep abdominal muscles as well as help build a better PF awareness.
This is a basic look at how the pelvic floor interacts with our diaphragm and abdominal muscles. This interaction is affected by changes in our posture and by external loading challenges. Both will affect the tone and pressure control of the system. Coordination and control of the entire system is the end game, not isolated work on the pelvic floor.
The good news is that you can start making changes to your pelvic floor control by working on your breathing. There is promising research that supports the training of breathing mechanics as the initial intervention vs skipping straight to doing kegels. Additionally, if there isn’t an understanding of what ALL the components of the abdominal canister are doing (is the diaphragm able to expand and contract fully? Are the abdominals over-recruited and putting excess strain on the system?) then it’s likely not the best course of action to jump straight into pelvic floor maximal contractions.
I want to say here that ITS OK not to know what all of this is doing! It’s ok to get this point in reading and go I HAD NO IDEA!! Seriously, that’s how I felt when I was introduced to all of this. But, now we know that there is more to the puzzle and that this blog post is meant for initial education. The next step is looking to your community for additional help.
1. Search out a pelvic health physiotherapist! Having a pelvic health physio on your side is wonderful. They are able to do internal exams (if that is something that you are comfortable consenting to) to understand exactly what the pelvic floor is doing at rest and with conscious effort. They address many pelvic floor concerns such as pain, prolapse, incontinence among other things. They will also guide the start to your movement journey and give you safe parameters to move forward on your individual goals.
2. Find a pilates instructor! My job as a pilates instructor/kinesiologist is to help people to move better and with more awareness. What I have found through all of the research is that Pilates and it’s principles, are very complimentary to pelvic floor rehabilitation. Proper breath support, building efficient movement patterns and understanding the necessary force generation for the loaded task is all worked on in pilates sessions. Many of us work closely with physiotherapists and other practitioners to support the transition from rehab movement to activity and sport.
Here are some of the fabulous Vancouver practitioners that I would recommend to reach out to:
The Cheerful Pelvis https://thecheerfulpelvis.com/
Rae Physiotherapy https://www.raephysiotherapy.com/
Envision Physiotherapy https://www.envisionphysio.com/
Pilates Process Vancouver https://www.pilatesprocess.ca/vancouver-studio/
Foundation Pilates https://foundationreformerpilates.com/
Mama Method https://www.mamamethod.ca/
Align Method https://www.alignmethod.ca/
Other Resources:
The Vagina Coach https://www.vaginacoach.com/
Julie Weibe https://www.juliewiebept.com/
References
About the Guest Author
Tiffany Johns is in constant motion. A former professional ballet dancer, she fell into pilates on a search for a better way to manage her dance injuries. This eventually led to her certifying in the Pilates Process Method. She is now an Instructor Trainer for Pilates Process as well as a registered Kinesiologist in BC. She graduated from UBC with her Bachelor of Kinesiology in 2018. She owns Pilates Process Vancouver and teaches private and group sessions as well as workshops and Teacher Training. She is continually curious about pelvic health and is passionate about education on this topic. She is a mother of two very active girls age 3 and 5. She loves to run and bike, and has recently fallen in love with olympic weightlifting.
Sorry, the comment form is closed at this time.